Digital Pharmacist Digest - 🔁 AI's Future in Medicine, Interoperability across EHR platforms, and more
17th August, 2023
Kevin Sam
3 min read
Hiya 👋
We’re back with another edition of the digital pharmacist digest!
Here are this week's links that are worth your time.
Are you enjoying this digest? It would mean a lot if you'd consider forwarding it on to someone that you think would also appreciate it!
Thanks for reading,
Kevin
📖What I'm reading
🤖 Artificial Intelligence and 🩺💻 Health informatics - Creation and Adoption of Large Language Models in Medicine
“Current evaluations of LLMs also do not quantify the benefits of novel collaboration between humans and artificial intelligence that is at the core of using these models in clinical settings. The methods for evaluating LLMs in the real world remain unclear. Concerns with current evaluations range from training dataset contamination (such as when the evaluation data are included in the training dataset) to the inappropriateness of using standardized examinations designed for humans to evaluate the models….
The purported benefits need to be defined and evaluations conducted to verify such benefits. Only after these evaluations are completed should statements be allowed such as an LLM was used for a defined task in this specific workflow, it measured a metric, and observed an improvement (or deterioration) in a prespecified outcome. Such evaluations also are necessary to clarify the medicolegal risks that might occur with the use of LLMs to guide medical care, and to identify mitigation strategies for the models’ tendency to generate factually incorrect outputs that are probabilistically plausible (called hallucinations).”
🤖 Artificial Intelligence and 🩺💻 Health informatics - Steering AI’s Future in Medicine
"Recognizing this potential, we should strive to equip our workforce with these transformative tools. The question now is: How do we do this responsibly? What might the “rules of the road” for AI look like in medicine? Below is a starting framework...
Rule No. 1: Safety First. There are hundreds of AI models out there, each built differently and structured to do different tasks. We need rigorous and consistent ways of testing these models to verify that they not only deliver on intended benefits but uphold patient safety at every step. This includes data privacy and security, which are non-negotiable. AI models must be hardwired to protect patient data from breaches or potential misuse in every scenario–from how data is accessed for analysis to how results are presented.
Rule No. 2: Transparency. Ultimately, AI will be adopted at the speed of trust, and that demands transparency. AI models must be open for meaningful inspection. Their decision-making should be replicable and their recommendations retraceable to a real-world medical source. For reasons I don’t need to explain, AI "hallucinations"— scenarios where LLMs fabricate confident, yet incorrect, answers—are unacceptable in the medical setting.
Rule No. 3: No Impaired Driving. We must train AI models on datasets that accurately reflect our diverse patient populations, regularly evaluate models for biases, and take corrective action if bias is detected. Moreover, as AI assumes increasingly complex tasks in healthcare, having a "driver" – a human decision-maker – in the seat is crucial. AI should act as a supportive tool, supplementing, not supplanting, the judgment of medical professionals.
Rule No. 4: They Need to Work. AI models must be more than technically sound; they must provide clinically relevant and actionable insights. To avoid exacerbating the "EHR alert fatigue" clinicians currently face from numerous irrelevant health record system alerts, AI models must not merely add to the noise. Instead, they should deliver precise, valuable information that genuinely contributes to data-driven healthcare. This will require AI models that can see the big picture and work seamlessly across diverse data types and timelines to help clinicians achieve superior outcomes for their patients."
🩺💻 Health informatics - JAMIA Study Reports 22-68% Interoperability Across EHR Platforms: 7 Implications
"A recent study of EHR interoperability found that 68% of data was “understood” when exchanged across different sites using the same vendor, but only 22% was “understood” when exchanged across different EHR vendors.
In the U.S., there are many companies developing workarounds to the perceived weaknesses of EHRs. Exchange-based interoperability is improving thanks to innovations like HL7 FHIR,
However we jointly believe that a rather different approach, built around standards-based data platforms, would be the ideal solution to deliver a seamless patient-centric digital experience for clinicians and patients.
openEHR (pronounced “open air”) pioneered this new approach and is gaining traction in Europe, but seems unlikely to gain adoption in the market-based U.S. health care system. EHR switching costs are VERY high.
It is a set of open specifications and free, standardized clinical data components designed explicitly to support the data platform approach, separating applications from data and storing the patient data in specialized datastores called “clinical data repositories” (CDRs)."
🩺💻 Health informatics - National Healthcare Interoperability Plan
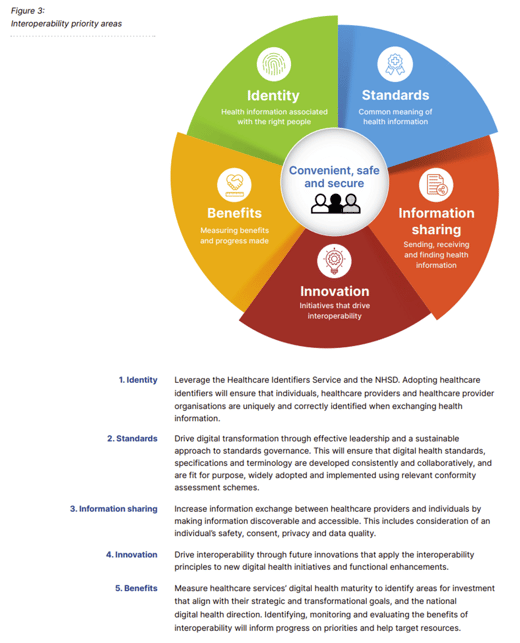
The Interoperability Plan identifies five priority areas to advance digital health interoperability in Australia. These building blocks will contribute to the National Digital Health Strategy’s interoperability objective
Did you find this article useful? If so, please consider forwarding this newsletter on to your colleagues.
Stay up-to-date with the Digital Pharmacist Digest
Any comments provided are personal in nature and do not represent the views of any employer